Managing dental extractions in patients with a history of cardiac surgery and ongoing anticoagulant or antiplatelet therapy requires careful planning, scientific understanding, and collaboration with medical specialists. The goal is to ensure patient safety by balancing two risks: bleeding complications during or after the procedure versus the far more dangerous risk of thrombosis (stroke, myocardial infarction) if anticoagulant therapy is improperly interrupted.
This essay explores the precautions, investigations, and protocols essential when performing a dental extraction on a patient who had coronary artery bypass graft (CABG) surgery and is currently taking blood-thinning medications.
Importance of Preoperative Assessment
Before proceeding with any invasive dental procedure, a thorough preoperative evaluation is mandatory. Patients who have undergone CABG surgery often remain on long-term medications such as aspirin, clopidogrel, warfarin, or newer oral anticoagulants (NOACs like apixaban or rivaroxaban). These drugs reduce the risk of thrombotic events but increase the risk of surgical bleeding.
Medical Consultation is the first critical step. Dentists must obtain clearance from the patient’s cardiologist or physician. Understanding the patient’s cardiac function, current medications, and overall risk factors helps in creating an individualized treatment plan.
Additionally, dentists should obtain a full medication history, including any blood thinners, antihypertensives, or diabetic medications, and evaluate any history of recent cardiovascular events. Stress-reduction strategies such as short morning appointments and sedation (if necessary) should also be considered to avoid cardiovascular stress during the procedure.
Recommended Blood Investigations
Specific laboratory investigations are crucial to assess bleeding risk and systemic stability:
| Test | Purpose | Scientific Reason |
|---|---|---|
| Complete Blood Count (CBC) | To check hemoglobin, total leukocyte count (WBC), and platelet count | – Anemia could worsen heart strain. – Low platelets can increase bleeding risk. – Infection signs (high WBCs). |
| Bleeding Time (BT) and Clotting Time (CT) | To check basic clotting ability | – Quick, simple screening for clotting disorders. |
| Prothrombin Time (PT), International Normalized Ratio (INR) | To assess extrinsic clotting pathway, especially if patient is on warfarin or anticoagulants | – INR should ideally be between 2.0–3.0 for minor oral surgery. – If >3.5, extraction should be deferred or adjusted. |
| Random Blood Sugar (RBS) / Fasting Blood Sugar (FBS) | To check glucose levels | – Uncontrolled diabetes slows healing and increases infection risk. – Many cardiac patients also have diabetes. |
| Serum Creatinine and Blood Urea (optional if patient has kidney issues) | To assess kidney function | – Important because long-term cardiac patients can have kidney dysfunction from medications or disease itself. |
By evaluating these parameters, dentists can predict and prepare for potential bleeding, delayed healing, or infection complications.
Management of Blood Thinners During Dental Extractions
One of the most common clinical dilemmas is deciding whether to continue or discontinue blood thinners before a dental extraction.
Antiplatelet Therapy (Aspirin, Clopidogrel)
Modern guidelines recommend that aspirin and clopidogrel should not be stopped for minor oral surgical procedures such as simple tooth extractions. Discontinuing these drugs significantly increases the risk of catastrophic thromboembolic events like myocardial infarction and stroke, often outweighing the manageable risk of bleeding.
Bleeding associated with antiplatelet drugs is usually minor and can be controlled with local measures such as pressure application, suturing, and hemostatic agents.
Anticoagulant Therapy (Warfarin, NOACs)
Patients on warfarin therapy require special attention to their INR levels:
- INR ≤ 3.0: Extraction can usually proceed safely with local hemostatic measures.
- INR > 3.5: The procedure should be postponed, or the warfarin dose may need adjustment under medical supervision.
For patients on newer anticoagulants (e.g., apixaban, rivaroxaban), minor dental procedures can typically be performed 12–24 hours after the last dose, timing the surgery during the drug’s lowest concentration (“trough levels”). However, coordination with the prescribing physician is essential.
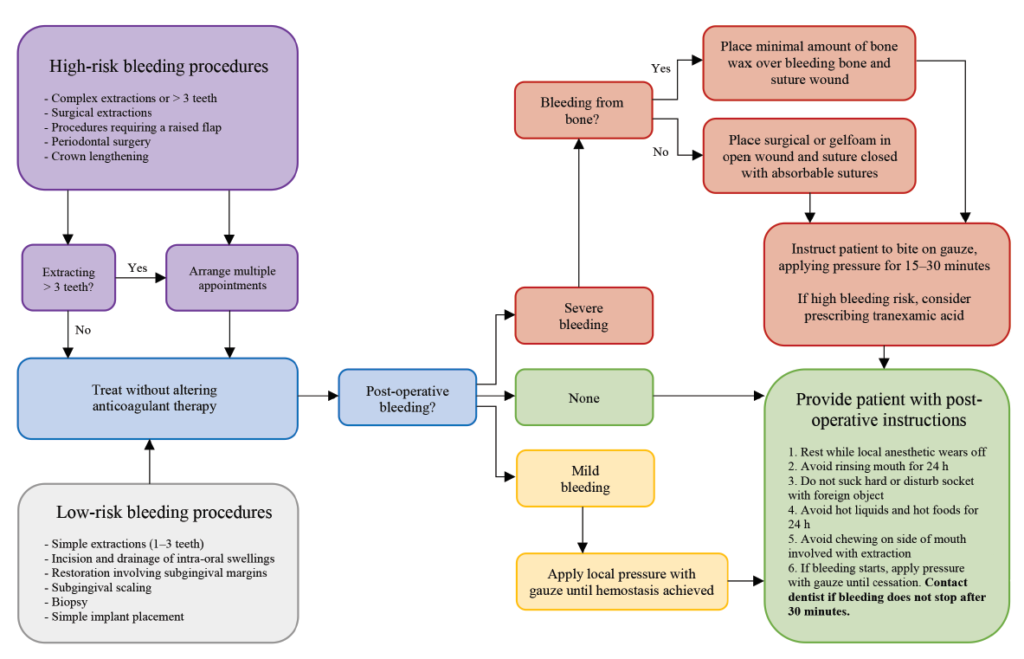
Overall, routine stoppage of anticoagulants is discouraged, and careful local management of bleeding is preferred.
| Drug | Stopping Before Extraction? | How Many Days to Stop (if absolutely necessary)? |
|---|---|---|
| Aspirin alone | No | — |
| Aspirin + Clopidogrel (dual therapy) | No | — |
| Warfarin | No if INR <3.0 | If INR >3.5, adjust under doctor’s advice (might stop for 2–3 days) |
| DOACs (e.g., Apixaban) | Usually not | Delay extraction for 12–24 hrs after last dose if needed |
Extraction Technique and Intraoperative Precautions
Sample Antibiotic Prophylaxis Regimen
When needed (i.e., if the patient is at risk for infective endocarditis — depends on cardiologist advice):
| Situation | Regimen |
|---|---|
| Standard Prophylaxis | Amoxicillin 2g orally 30–60 minutes before the procedure |
| If allergic to penicillin | Clindamycin 600mg orally 30–60 minutes before the procedure |
Stress Reduction
A stress-free environment is vital. Morning appointments, a calm setting, and clear communication help reduce patient anxiety and avoid cardiac stress responses.
Anesthesia Considerations
Local anesthesia containing vasoconstrictors (e.g., epinephrine) can be used, but in minimal effective concentrations (e.g., lidocaine 2% with 1:200,000 epinephrine). Careful aspiration is necessary to avoid intravascular injection, which could cause tachycardia and hypertension.
Atraumatic Extraction
The extraction should be performed with minimal trauma:
- Use elevators and forceps gently.
- Avoid excessive manipulation of soft tissue or bone.
Local Hemostasis
Effective intraoperative bleeding control includes:
- Placement of a collagen sponge, oxidized cellulose (e.g., Surgicel), or gelatin sponge (e.g., Gelfoam) into the socket.
- Primary suturing of the socket, if necessary.
- Application of pressure packs for at least 45 minutes post-extraction.
Tranexamic acid mouth rinses (5%) are also highly effective at promoting clot stability and reducing postoperative bleeding.
Postoperative Care and Patient Instructions
After the procedure:
- The patient should maintain pressure over the extraction site using a gauze pack.
- No spitting, mouth rinsing, or use of straws for the first 24 hours to protect the forming clot.
- A soft, cool diet should be followed, avoiding hard or hot foods.
- If bleeding persists beyond 6–8 hours despite pressure, the patient should return for reassessment.
Pain Management should prioritize non-NSAID options like paracetamol unless otherwise guided by the physician, as NSAIDs can further impair platelet function and increase bleeding.
Conclusion
Dental extraction in patients with a history of cardiac disease and who are under anticoagulant or antiplatelet therapy is safe when done with careful planning. Stopping blood thinners carries a significant risk of thrombosis and life-threatening events. Therefore, in most cases, dental extractions can and should be performed without discontinuing these medications, while focusing on effective local hemostatic measures and close collaboration with the patient’s physician.
Understanding the scientific rationale, following standardized protocols, and maintaining vigilant perioperative care can help dental professionals manage these complex patients safely and effectively, ensuring both successful dental outcomes and patient systemic health.
To know more about the correlation between cardiac health and oral healthcare, click here: https://flossdaily.in/heart-health-oral-care
Soruces:
- https://www.ada.org/resources/ada-library/oral-health-topics/oral-anticoagulant-and-antiplatelet-medications-and-dental-procedures
- https://www.sdcep.org.uk/media/ypnl2cpz/sdcep-management-of-dental-patients-taking-anticoagulants-or-antiplatelet-drugs-2nd-edition.pdf
- https://sites.uw.edu/anticoag/conditions/peri-procedural-anticoagulation/suggestions-for-anticoagulation-management-before-and-after-dental-procedures/
- https://pubmed.ncbi.nlm.nih.gov/?term=dental+extractions+anticoagulant+therapy
Disclaimer:
The information provided here is for informational purposes only. This may not cover everything about particular health conditions. For any unintentional inaccuracy in our content please contact us.

